 |
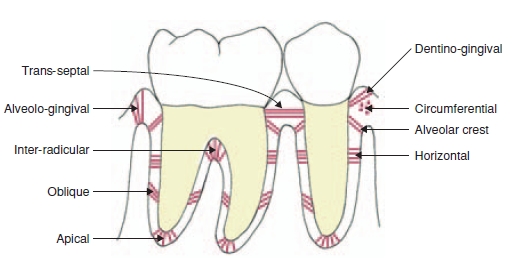
Periodontal Ligament Groups
The periodontal ligament, commonly abbreviated as the PDL, is a group of specialized connective tissue fibers that essentially attach a tooth to the alveolar bone within which it sits.
Features
Functions of PDL are supportive, sensory, nutritive, and remodeling.
The PDL substance has been estimated to be 70% water, which is thought to have a significant effect on the tooth's ability to withstand stress loads. The completeness and vitality of the PDL are essential for the functioning of the tooth.
The PDL ranges in width from 0.15 to0.38 with its thinnest part located in the middle third of the root.
The PDL is a part of the periodontium that provide for the attachment of the teeth to the surrounding alveolar bone by way of the cementum.
The PDL appears as the periodontal space of 0.4 to 1.5 mm on radiographs, a radiolucent area between the radiopaque lamina dura of the alveolar bone proper and the radioopaque cementum.
There are progenitor cells in the periodontal ligament that can differentiate into osteoblasts for the physiological maintenance of alveolar bone and, most likely, for its repair as well.
Structure
The PDL consist of cells, and extracellular compartment of fibers. The cells are fibroblast, epithelial cells, undifferentiated mesenchymal cells, bone and cementum cells. The epithelial rests of Malassez are also present; these groups of epithelial cells become located in the mature PDL after the disintegration of Hertwig epithelial root sheath during the formation of the root. The extracellular compartment consists of collagen fibers bundles embedded in intercellular substance. The PDL collagen fibers are categorized according to their orientation and location along the tooth.
Alveodental ligament
The main principal fiber group is the alveolodental ligament, which consists of five fiber subgroups: alveolar crest, horizontal, oblique, apical, and interradicular on multirooted teeth. Another principal fiber other than the alveolodental ligament are the transseptal fibers.
All these fibers help the tooth withstand the naturally substantial compressive forces which occur during chewing and remain embedded in the bone. The ends of the principal fibers that are within either cementum or alveolar bone proper are considered Sharpey fibers.
Alveolar crest fibers
Alveolar crest fibers (I) extend obliquely from the cementum just beneath the junctional epithelium to the alveolar crest. These fibers prevent the extrusion of the tooth and resist lateral tooth movements.
Horizontal fibers
Horizontal fibers (J) attach to the cementum apical to the alveolar crest fibers and run perpendicularly from the root of the tooth to the alveolar bone..
Oblique fibers
Oblique fibers (K) are the most numerous fibers in the periodontal ligament, running from cementum in an oblique direction to insert into bone coronally.
Apical fibers
Apical fibers are found radiating from cementum around the apex of the root to the bone, forming base of the socket or alveolus.
Interradicular fibers
Interradicular fibers are only found between the roots of multirooted teeth, such as premolars and molars. They also attach from the cementum and insert to the nearby alveolar bone.
Transseptal fibers
Transseptal fibers (H) extend interproximally over the alveolar bone crest and are embedded in the cementum of adjacent teeth; they form an interdental ligament. These fibers keep all the teeth aligned. These fibers may be considered as belonging to the gingival tissue because they do not have an osseous attachment.
Pathology
References
|
Dental Problems are the worst thing anybody could face. An overview on the latest and some of the best solutions available
Thursday, 26 September 2013
Understanding our Mouth -- The Periodontal Ligament
Subscribe to:
Post Comments (Atom)
No comments:
Post a Comment